Types of Incontinence
An involuntary leakage of urine1 is known as incontinence or bladder leakage.It can stop a man from living the active life he once lived and make him feel alone and isolated. For many men, leaking urine can mean embarrassment and feeling depressed.
There are different types of urinary incontinence:
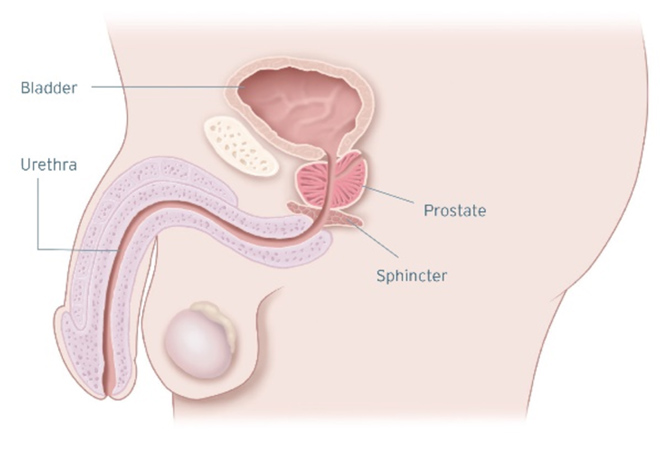
Stress Urinary Incontinence (SUI) occurs when physical movement or activity — such as coughing, laughing, sneezing, exercising or lifting something heavy — puts pressure or stress on a man’s bladder. It is usually caused by a damaged or weakened sphincter. When damaged, this muscle cannot squeeze and close off the urethra; the result is urine leakage. Stress urinary incontinence is not related to psychological stress. In men, the most common cause of stress urinary incontinence is the surgical removal of the prostate gland to treat prostate cancer. This procedure is called a prostatectomy.2,3
Urge Incontinence (also known as overactive bladder [OAB]) is diagnosed when a man has an overwhelming and sudden, intense need to urinate (gotta go, gotta go!) that may prevent reaching the toilet in time and an involuntary loss of urine. You may need to urinate often, including throughout the night. Causes of overactive bladder include damage to the bladder’s nerves, damage to other parts of the nervous system and damage to the muscles. Minor conditions, such as infection,4 or a more-severe conditions such as multiple sclerosis, Parkinson’s disease, diabetes and stroke can affect nerves and may lead to urge incontinence. 3,5
Mixed Incontinence is present when a man suffers from symptoms of both stress urinary incontinence and urge incontinence. A man has mixed incontinence if he leaks urine when he sneezes, coughs, laughs, exercises or lifts something heavy and leaks urine after a sudden urge to urinate, while he sleeps, after drinking water, or hearing or touching water. Mixed incontinence shares the causes of both SUI and urge incontinence.3,6
Overflow Incontinence. You experience frequent or constant dribbling of urine due to a bladder that doesn’t empty completely.4
Functional Incontinence. A physical or mental impairment keeps you from making it to the toilet in time. For example, if you have severe arthritis, you may not be able to unbutton your pants quickly enough.4
Treatment options range from behavioural modifications to invervention and external devices, injections and long-term options like the male sling or artificial urinary sphincter.
Take the Quiz
Take our quiz to identify if you are experiencing urinary incontinence symptoms and help kick-start the conversation with your doctor.
Questions to Ask
Helpful hints on how to start the conversation with your GP or urologist, and other useful resources.
References
- Chapple C, Milsom I. Urinary incontinence and pelvic prolapse epidemiology and pathophysiology. In: Wein AJ, Kavoussi LR, Novick AC, et al. (eds). Campbell-Walsh Urology. 10th ed. Philadelphia, PA: WB Saunders Elsevier; 2012:1871-95.
- Stress Incontinence. Mayo Clinic Website. http://www.mayoclinic.org/diseases-conditions/stress-incontinence/basics/definition/con-20027722. Accessed 26 November 2019
- Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213-40.
- Urinary incontinence - Symptoms and causes - Mayo Clinic Website. https://www.mayoclinic.org/diseases-conditions/urinary-incontinence/symptoms-causes/syc-20352808.Accessed 26 November 2019
- Types of Urinary Incontinence. WebMD Website. http://www.webmd.com/urinary-incontinence-oab/types-of-urinary-incontinence. Accessed September 13, 2016.
- Mixed Incontinence. WebMD Website. http://www.webmd.com/urinary-incontinence-oab/mixed-incontinence. Accessed September 13, 2016.
Results from case studies are not necessarily predictive of results in other cases. Results in other cases may vary. All images are the property of Boston Scientific. All trademarks are the property of their respective owners.
Disclaimer: Individual symptoms, situations, circumstances and results may vary. This information is not intended to be used for medical diagnosis or treatment or as a substitute for professional medical advice. Please consult your doctor or qualified healthcare provider regarding your condition and appropriate medical treatment.
These Videos are meant for informational purposes only and may not be indicative of clinical outcome. The opinions, procedures and patient care policies expressed or depicted in the videos are those of the physician or practice nurse and do not necessarily reflect the opinions, policies or recommendations of Boston Scientific Corporation or any of its employees.
This site is intended for Australian residents only. Please review the Boston Scientific Privacy Policy, for practices on the collection, storage, use and disclosure of your personal information.
CAUTION : Indications, contraindications, warnings and instructions for use can be found in the product labelling supplied with each device.